Certified Primary Stroke Center
Beebe Healthcare, as a certified Primary Stroke Center, is recognized by emergency medical personnel as a hospital of choice in a stroke emergency and provides a nationally recognized standard of care that fosters the best possible outcomes for stroke patients.
Beebe Healthcare provides both inpatient (in the hospital at the Margaret H. Rollins Lewes Campus) and outpatient (in a private practice setting) neurology services.
Download: Know the Signs of Stroke
Outpatient Neurology for Our Community
Beebe Healthcare's outpatient neurology physicians and providers work with a broad variety of patients - from those recovering from stroke to those who experience headaches/migraines, seizures, and more. Here are some of the medical concerns treated by Beebe neurologists:
- Stroke
- Seizures and epilepsy
- Headaches and migraines
- Multiple sclerosis (MS)
- Parkinson’s disease
- Alzheimer’s disease and memory loss
How We Diagnose and Treat a Stroke
During stroke, time lost is brain lost. A stroke happens when blood flow to the brain is disrupted, either by a bleed or a clot. The longer a stroke continues, the more damage to brain. That's why it's said that during a stroke, time lost is brain lost. Clots cause most strokes. For these, a drug called tissue plasminogen activator (tPA) can break up the clot and stop a stroke in its tracks—but the drug needs to be given within a certain window of time.
Because a stroke interferes with the supply of oxygen to the brain, damage may occur that impacts the body’s ability to function as it did before. The patient’s subsequent disability depends upon where the stroke occurred in the brain, what kind of stroke it was, how serious it was, and whether aggressive medication was given within the four-and-a-half-hour time window. Diagnostic tools such as a carotid duplex scan or a magnetic resonance angiogram or image (MRA or MRI) will show where the stroke occurred.
In many cases, a patient with a stroke comes into the hospital and receives immediate stroke care. During recovery, the patient then may work with a neurologist in an outpatient or practice setting. The patient likely also works with physical rehab teams during recovery.
Meet the Neurology Team
If you are trying to make an outpatient appointment with a neurologist, select providers who have an office location outside of the hospital. These providers include: Dr. Ionita, Dr. Peet, Dr. Thomas.
Stroke Support Group - Beebe Partnership with Jefferson Health
Second Tuesday of each month
Due to COVID-19, the Stroke Support Group will join up with Jefferson's Stroke Support in order to host regular virtual meetings. Jefferson Health Stroke Support Group meets the second Tuesday of the month at 2 p.m. via Zoom. First, download the Zoom app to your smartphone or computer. Then sign up for the Jefferson group via facebook.com/farberneuro and look under Upcoming Events. You can also email [email protected] for the information and link to the Zoom meeting. Or, click this link: https://Jefferson.zoom.us/meeting/register/tJ0oce6pqjgqEtxSqSlo4Vhci75kfdIadBO0. The Jefferson stroke support group provides a safe space to connect with other stroke survivors and those caring for or living with a person who has experienced a stroke. The group is led by experts from the Vickie and Jack Farber Institute for Neuroscience and provides emotional and practical support. Patients, families and friends are all invited to attend free of charge. Each month there will be a brief presentation at the beginning of the meeting that focuses on a topic related to stroke. If you need additional support from Beebe, contact Bobbi-Lynn Hensey, BSN, RN, CCRN, Stroke Program Coordinator at Beebe at (302) 645-3227.
Commonly Asked Questions
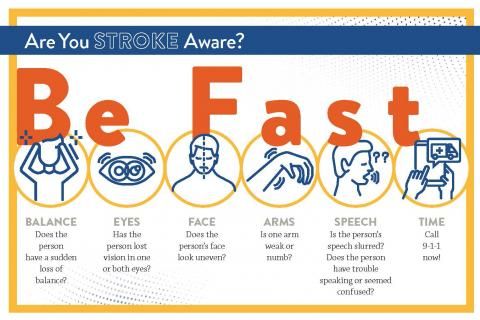
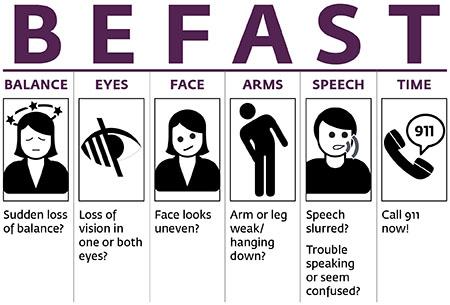
Know the signs of stroke. Use the BE FAST method and call 911 if you suspect a stroke.
You can memorize the signs of stroke through the acronym BE FAST:
- Balance. Is there a sudden loss of balance or coordination?
- Eyes. Is there sudden blurred vision or other vision trouble?
- Face. Ask the person to smile. Is one or both sides of the face drooping?
- Arms. Ask the person to raise both arms. Does one side drift downward?
- Speech. Does the person have slurred or garbled speech?
- Time. Time to call 911 for immediate help if you notice any of these signs.
Those with the following symptoms are at higher risk for a stroke:
- High Blood Pressure
- Heart Disease
- Diabetes
- Atrial Fibrillation
- Lifestyles
- Smoking
- Obesity
- Sedentary
- Alcohol consumption
- Transient Ischemic Attack (TIA)
- Sudden numbness or weakness of face, arm, or leg — especially on one side of the body
- Sudden confusion, trouble speaking or understanding
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, dizziness, loss of balance or coordination
- Sudden severe headache with no known cause
Source: National Institute of Neurological Disorders and Stroke & National Stroke Association